Receiving an MRI report can be stressful. Many patients walk into a clinic anxious after reading terms like disc bulge, degeneration, nerve compression, or spondylosis. The fear is understandable — but the truth is, not every abnormal MRI finding is dangerous or requires surgery.
As a neuro surgeon in Bangalore, one of the most common questions we hear is:
“Doctor, my MRI looks bad — do I need surgery?”
In this article, based on real clinical experience and the insights shared in the video, we explain what MRI scan results actually mean, how a spine surgeon interprets them, and when treatment is necessary versus when reassurance is enough.
MRI Scan Results Explained
ㆍMRI reports often look alarming, but most findings are not dangerous.
ㆍCommon terms like disc bulge or degeneration are frequently age-related and may not cause pain.
ㆍSymptoms matter more than the MRI report when deciding treatment.
ㆍMost spine problems do not need surgery and improve with conservative care.
ㆍAn experienced neuro surgeon in Bangalore can clarify findings and prevent unnecessary procedures.
What Is an MRI Scan and Why Is It Ordered?
MRI (Magnetic Resonance Imaging) is a highly detailed imaging test used to visualize the brain, spine, spinal cord, discs, and nerves.
Doctors usually recommend an MRI when patients have:
ㆍPersistent neck or back pain
ㆍPain radiating to arms or legs
ㆍNumbness, tingling, or weakness
ㆍHeadaches, dizziness, or seizures
ㆍSuspected nerve compression or spinal cord problems
MRI scans show structure, not pain. This distinction is extremely important.
Why MRI Reports Often Look Scary (But Aren’t Always)
MRI reports are written in technical medical language, not patient-friendly terms. Words like:
ㆍDisc bulge
ㆍDisc degeneration
ㆍMild compression
ㆍReduced disc height
sound alarming but are often age-related or incidental findings.
Common MRI Findings Explained Simply
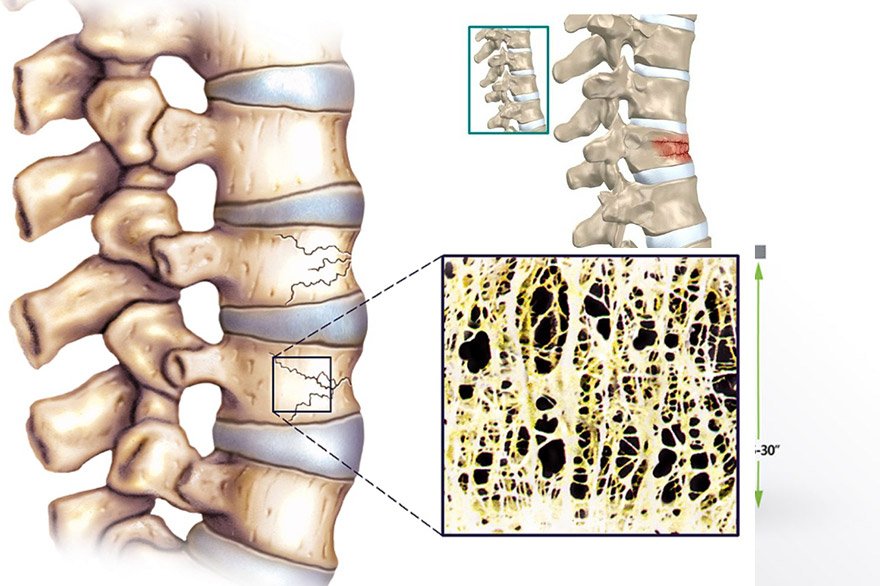
1. Disc Bulge or Disc Protrusion
A disc bulge means the disc has slightly extended beyond its normal boundary.
✔ Very common
✔ Often age-related
✔ Frequently asymptomatic
A spine surgeon looks at:
ㆍSeverity
ㆍNerve involvement
ㆍPatient symptoms
Not every disc bulge causes pain or needs treatment.
2. Disc Degeneration
Disc degeneration means gradual wear and tear of spinal discs.
✔ Part of natural aging
✔ Seen even in people without pain
✔ Not an emergency finding
Degeneration alone does not mean surgery.
3. Nerve Compression
This finding needs closer attention.
If nerve compression correlates with:
ㆍArm or leg pain
ㆍNumbness
ㆍWeakness
then treatment may be required — but even here, surgery is not always the first option.
4. Mild Spinal Canal Narrowing
“Mild” narrowing rarely needs surgery. Many patients improve with:
ㆍPhysiotherapy
ㆍMedications
ㆍLifestyle modification
A neuro clinic in Bangalore with spine expertise focuses on conservative care first whenever possible.
Why Symptoms Matter More Than the MRI Report
One of the most important principles in neurosurgery is:
We treat the patient, not the MRI.
Two patients can have the same MRI report:
ㆍOne may have severe pain
ㆍThe other may have none
A qualified neuro surgeon in Bangalore always correlates:
ㆍMRI findings
ㆍClinical symptoms
ㆍNeurological examination
This prevents unnecessary procedures and anxiety.
When MRI Findings Do Need Serious Attention
You should seek urgent specialist evaluation if MRI findings are associated with:
ㆍProgressive weakness in arms or legs
ㆍLoss of balance or coordination
ㆍBowel or bladder control issues
ㆍSevere spinal cord compression
ㆍBrain lesions with neurological symptoms
In such cases, early treatment can prevent permanent nerve damage.
Do All MRI Abnormalities Require Spine Surgery?
No. In fact, most do not.
Studies and clinical experience show that:
ㆍOver 70–80% of spine-related problems improve without surgery
ㆍConservative treatment is effective in most cases
Surgery is considered only when:
ㆍSymptoms worsen despite treatment
ㆍNeurological deficits progress
ㆍQuality of life is severely affected
A responsible spine surgeon will always explain all options clearly.
How a Neuro Clinic in Bangalore Evaluates MRI Reports
At a specialized neuro clinic in Bangalore, MRI evaluation involves:
ㆍDetailed symptom history
ㆍPhysical and neurological examination
ㆍCorrelation with imaging
ㆍDiscussion of treatment options
This approach ensures:
ㆍAccurate diagnosis
ㆍAvoidance of overtreatment
ㆍPatient confidence and clarity
Treatment Options After MRI Evaluation
Depending on findings and symptoms, treatment may include:
ㆍMedications for pain and inflammation
ㆍPhysiotherapy and posture correction
ㆍLifestyle modifications
ㆍTargeted injections (in selected cases)
ㆍSurgery (only when clearly indicated)
Each plan is individualized, not MRI-driven alone.
Why Getting the Right Opinion Matters
Many patients panic after reading MRI reports online or receiving incomplete explanations. A second opinion from an experienced neuro surgeon in Bangalore often reveals:
ㆍSurgery is not needed
ㆍSymptoms are manageable
ㆍRecovery is achievable with conservative care
Clarity reduces fear — and fear itself worsens pain.
When Should You Consult a Specialist?
Confused or Worried After Seeing Your MRI Report?
If your MRI scan is causing anxiety or symptoms are affecting daily life, expert neurological evaluation can provide clarity and reassurance.
Consult an experienced Neuro Surgeon in Bangalore
Visit a trusted Neuro Clinic in Bangalore Get guidance from a qualified Spine Surgeon
Available at Jayanagar & Electronic City
Conclusion
MRI scans are powerful diagnostic tools, but they do not tell the whole story. Abnormal findings are common and often harmless. What truly matters is how those findings relate to your symptoms and neurological health.
Before assuming the worst, speak with an experienced neuro surgeon in Bangalore who can interpret your MRI in the right clinical context. In most cases, reassurance and conservative care are all that is needed.
FAQs
What should I do if my MRI report looks abnormal?
Consult a neuro surgeon or spine specialist who can correlate findings with symptoms before deciding on treatment.
Can MRI reports be misleading?
Yes. MRI shows structural changes, many of which are normal age-related findings and may not cause pain.
Do disc bulges always require surgery?
No. Most disc bulges are treated successfully without surgery.
When is spine surgery actually required?
Surgery is considered only when neurological deficits worsen or conservative treatment fails.
Should I get a second opinion for MRI findings?
Yes. A second opinion from a qualified neuro surgeon in Bangalore often prevents unnecessary treatment.