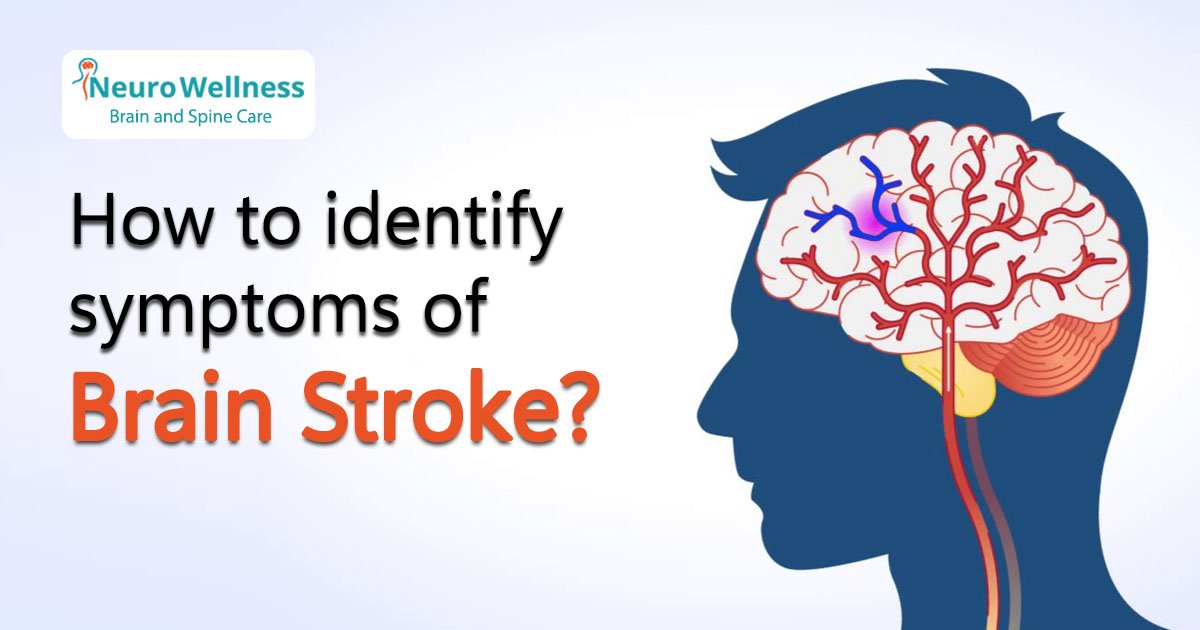
Imagine someone suddenly struggling to smile or speak — their face droops on one side, and their words come out garbled. This isn’t just fatigue or confusion — it could be a stroke. A stroke is a medical emergency that occurs when blood flow to the brain is interrupted, and every second counts. Recognizing the early warning signs can save lives and significantly reduce long-term disability. In this article, you’ll learn how to identify the most common — and sometimes subtle — signs of stroke.
Common Warning Signs of Stroke
Medical experts use the acronym F.A.S.T. to help people quickly remember the most urgent symptoms of a stroke:
• F – Face Drooping: Ask the person to smile. Does one side of their face droop or feel numb?
• A – Arm Weakness: Ask them to raise both arms. Is one arm drifting downward or feeling weak?
• S – Speech Difficulty: Ask them to repeat a simple sentence. Is their speech slurred or strange?
• T – Time to Call Emergency Services: If you see any of these signs, call emergency services immediately.
But F.A.S.T. doesn’t cover all symptoms. Doctors now recommend the B.E.F.A.S.T. approach to catch more signs:
• B – Balance: Sudden loss of balance or coordination, often with dizziness.
• E – Eyes: Sudden blurred or double vision in one or both eyes.
Together, B.E.F.A.S.T. provides a more complete picture of what to watch for — especially in strokes that affect the brain’s back side (posterior circulation), which may not show facial symptoms.
What to Do If You Suspect a Stroke
If you notice any of the above symptoms — even if they go away within minutes — do not ignore them. Immediate action can mean the difference between full recovery and lifelong disability.
Here’s what to do:
1. Call Emergency Services Immediately: Do not wait. The faster a stroke victim receives medical care, the better the chances of recovery.
2. Note the Time of Symptom Onset: Doctors need this to determine treatment options like clot-busting medications.
3. Do Not Give Food or Water: The person may have difficulty swallowing, which increases the risk of choking.
4. Keep the Person Calm and Still: Avoid unnecessary movement until help arrives.
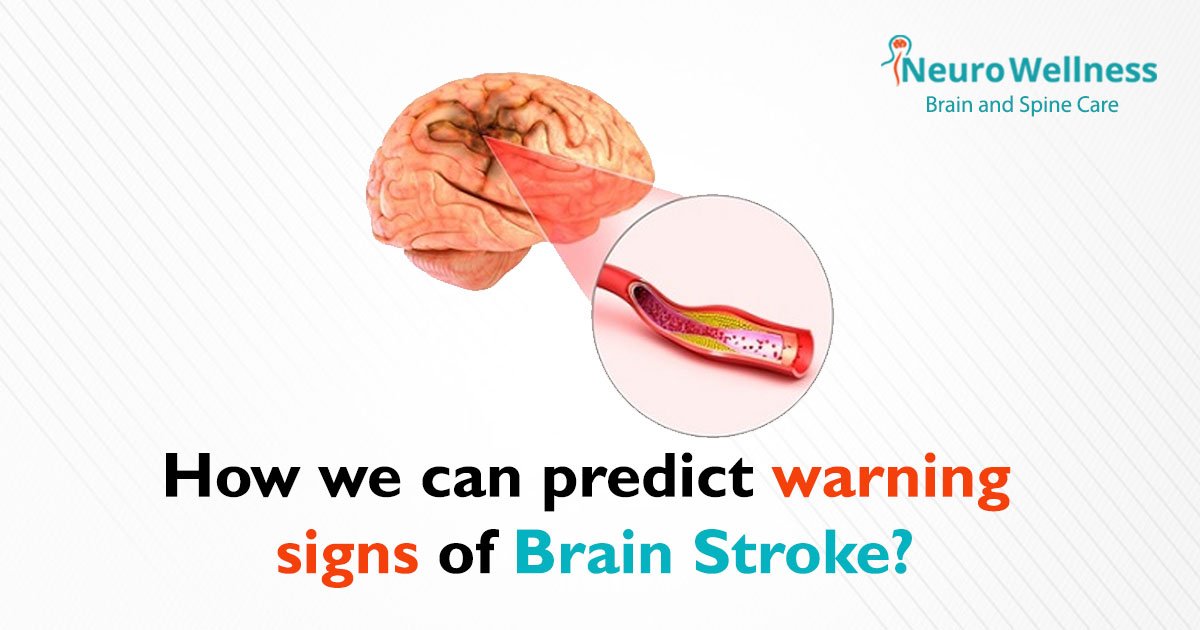
Types of Stroke (and Why They Matter)
Understanding the types of strokes can help explain why symptoms vary:
1. Ischemic Stroke (most common – ~87%): Caused by a blockage in an artery supplying blood to the brain.
2. Hemorrhagic Stroke: Caused by bleeding into the brain due to a ruptured vessel.
3. Transient Ischemic Attack (TIA) or Mini-Stroke: Temporary blockage with stroke-like symptoms that resolve in minutes to hours. It’s still an emergency and a warning sign of a future major stroke.
Stroke Risk Factors & Prevention Tips
Common Risk Factors:
• High blood pressure (most important)
• Diabetes
• Smoking
• High cholesterol
• Obesity
• Sedentary lifestyle
• Atrial fibrillation (irregular heartbeat)
• Family history of stroke
How to Lower Your Risk:
• Monitor your blood pressure and keep it under control.
• Exercise regularly – even 30 minutes of brisk walking helps.
• Eat a balanced diet rich in fruits, vegetables, and whole grains.
• Quit smoking and avoid excessive alcohol.
• Manage stress through mindfulness or yoga.
• Regular checkups, especially after age 40 or with a family history of stroke.
Conclusion: Early Detection Saves Lives
Strokes can strike anyone, anytime — but recognizing the warning signs early can mean faster treatment, better recovery, and even saved lives. Whether it’s sudden dizziness, slurred speech, or facial drooping, every second counts.
If you or a loved one experience any symptoms of stroke, don’t wait — seek immediate medical help.
Worried about your risk of stroke?
Book a consultation with our top neurologists at Neurowellness Brain & Spine Clinic, Bangalore.
We offer expert evaluation, personalized risk assessments, and preventive care to keep your brain healthy.
FAQs
1. Can stroke symptoms go away on their own?
Yes, in the case of a Transient Ischemic Attack (TIA), symptoms may disappear within minutes or hours — but this is still a medical emergency and a warning sign of a future stroke.
2. Are stroke symptoms always sudden?
Most stroke symptoms occur suddenly. However, in some cases (like small vessel disease), symptoms may be more subtle and progress slowly.
3. Can younger people have strokes?
Absolutely. While risk increases with age, strokes can and do occur in people under 45 — especially those with risk factors like hypertension, diabetes, or lifestyle issues.
4. What tests are done to diagnose a stroke?
Common tests include CT scan, MRI, carotid ultrasound, and blood tests to identify the type and cause of the stroke.
5. Is full recovery possible after a stroke?
Yes, especially if treatment begins quickly. Recovery depends on the type of stroke, the severity, the area of the brain affected, and how quickly treatment begins.