Meningitis and amoebic encephalitis are among the deadliest brain infections worldwide. While meningitis still claims lives despite treatment, amoebic encephalitis (caused by Naegleria fowleri) has a mortality rate of over 90%. Both conditions progress rapidly, making early recognition and prevention critical for survival.
In this blog, Dr. Ganesh Veerabhadraiah, senior neurosurgeon at Neurowellness, explains the symptoms, risks, and preventive steps everyone should know.
The brain is the most fragile part of the body. It works like a command center, guiding how we move, talk, breathe, and think. It is protected by a clean fluid called cerebrospinal fluid (CSF) and strong coverings called meninges.
Normally, no bacteria or parasites should ever enter this space. But if they do, the results can be deadly.
How Dangerous Is Meningitis?
Warning Signs to Watch For
Why Are We Hearing About Kerala?
Recently, there have been reports of amoebic encephalitis in Kerala.
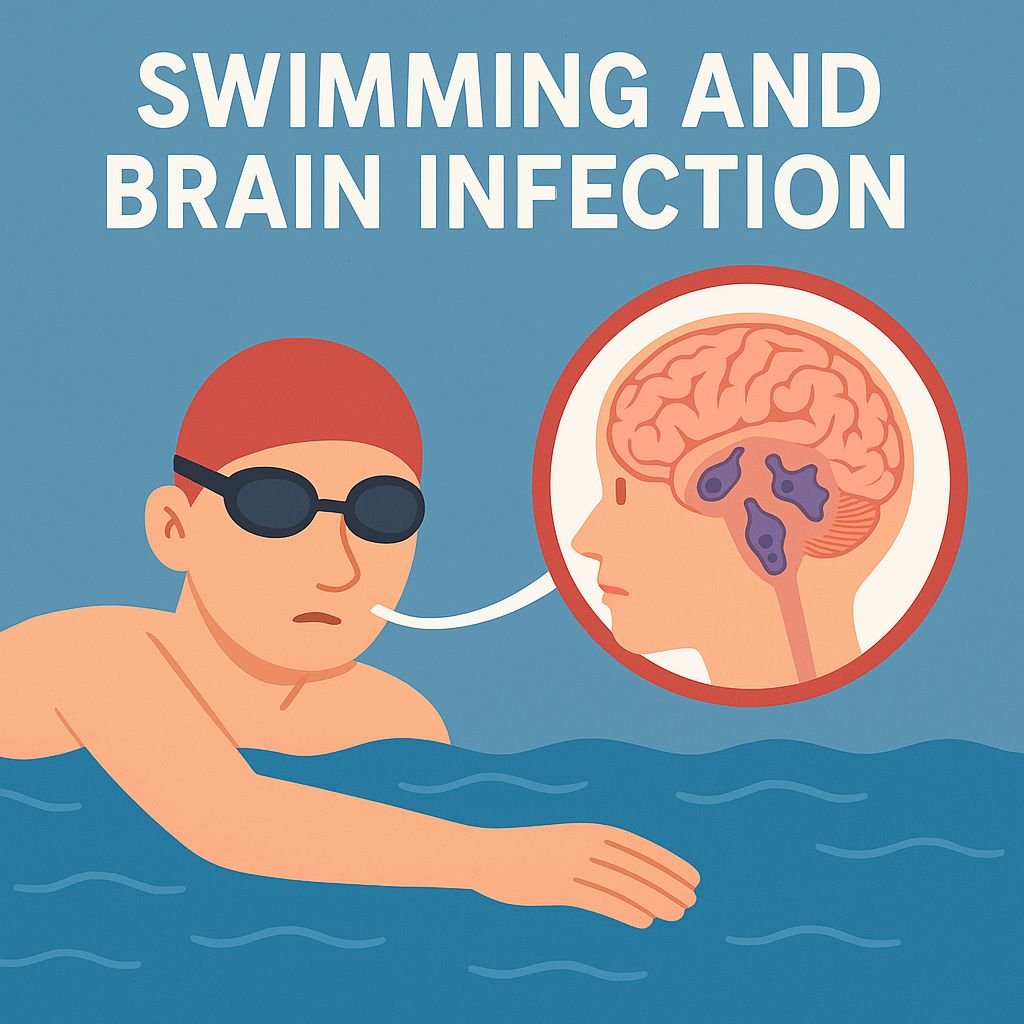
PAM is usually from exposure to unclean or poorly chlorinated water in ponds, lakes, and swimming pools.
When someone dives or swims in such water, the amoeba can enter through the nose. From there, it travels to the brain, causing severe swelling and inflammation. Sadly, most cases progress so fast that they are fatal within days of symptoms starting.
Who Is at Higher Risk?

Dr. Ganesh Veerabhadraiah
Consultant – Neurosurgeon, Neurointerventional Surgery, Spine Surgeon (Neuro)
23+ Years Experience Overall (17+ years as Neuro Specialist)
Available for Consultation: Jayanagar 9th Block & Kauvery Hospital, Electronic City
How Can We Protect Ourselves?
Conclusion
Meningitis and amoebic encephalitis are not rare health issues — they are global threats. With mortality rates as high as 25% for meningitis and 90% for amoebic encephalitis, prevention is the best protection.
✅ Choose safe water
✅ Recognize early warning signs
✅ Seek immediate medical care
Don’t wait until it’s too late. If you or a loved one shows symptoms of severe headache, seizures, or confusion,
FAQs
1) What are the first symptoms of meningitis?
Severe headache, vomiting, stiff neck, fever, confusion, and seizures are common warning signs.
2) How does amoebic encephalitis spread?
It spreads when contaminated water carrying Naegleria fowleri enters through the nose and travels to the brain.
3) Who is at higher risk of brain infections?
Children, elderly people, and those with weakened immunity (due to chronic illness, steroids, or cancer treatment) face higher risk.
4) Can meningitis and amoebic encephalitis be prevented?
Yes. Avoid unsafe water sources, swim only in chlorinated pools, and seek immediate medical help if symptoms appear.
5) What is the survival rate of amoebic encephalitis?
Unfortunately, more than 90% of patients do not survive, making prevention and rapid diagnosis essential.