Around 20% of stroke victims are between the ages of 20 and 55. Knowing the symptoms of a stroke and acting quickly can mean the difference between a life saved and a tragic outcome.
Stroke is the fifth leading cause of mortality in the United States, as well as the top cause of adult disability. According to the National Stroke Association, few people understand what a stroke is and how to spot it when it occurs.
Book a Consultation with our Stroke Specialists in Bangalore

What is a golden hour?
When someone is having a stroke, what we call “Golden Hour” can make all the difference in the world. The first 3.5 hours is crucial because stroke patients have a significantly better chance of surviving and avoiding long-term brain damage if they arrive at the hospital in right time and are treated with a clot bursting medicine known as TPA.
What is TPA?
TPA is a thrombolytic medication, also known as a “Clot Burster.” This clot burster is used to break up the clot that is causing a blockage or disruption in the flow of blood to the brain and aids in the restoration of blood flow to the affected part of the brain. It is administered intravenously (IV).

Dr. Ganesh Veerabhadraiah
Consultant – Neurosurgeon, Neurointerventional Surgery, Spine Surgeon (Neuro)
23+ Years Experience Overall (17+ years as Neuro Specialist)
Available for Consultation: Jayanagar 9th Block & Kauvery Hospital, Electronic City
Thrombolysis- A “clot burster” medicine
Ischaemic strokes are frequently treated with injections of alteplase, a medication that breaks blood clots and restores blood flow to the brain.
This application of “clot bursting” medication is known as thrombolysis.
Alteplase is most effective when administered as soon as possible after a stroke occurs – ideally within 4.5 hours.
It is not generally advised if more than 4.5 hours have passed, as it is unclear how effective it is after this period.
Before using alteplase, a brain scan must be performed to confirm the diagnosis of an ischemic stroke.
This is due to the fact that the medication has the potential to exacerbate the bleeding that happens in hemorrhagic strokes.
It is critical to seek therapy for Ischemic Stroke as soon as possible because we now have a clot burster called TPA (Tissue Plasminogen Activator). It’s an enzyme medicine that dissolves clots, and it may be given at only in stroke-ready(comprehensive stroke care)hospital.
What tests are required?
A CT scan of the brain will be performed as soon as possible to evaluate whether you or a family member can be offered TPA. This is to determine whether the stroke can be improved by TPA. If the stroke was caused by bleeding into the brain, TPA can exacerbate the hemorrhage. You will not be able to obtain TPA if this is the case. A blood test will also be performed to ensure that you do not have a bleeding disorder.
If the CT scan reveals no brain bleeding, doctors can employ the clot-dissolving medication TPA if specific criteria are met. This will be discussed with you by the doctor.
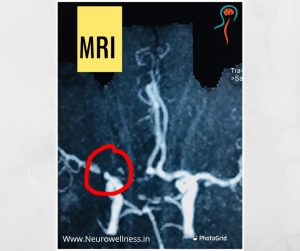
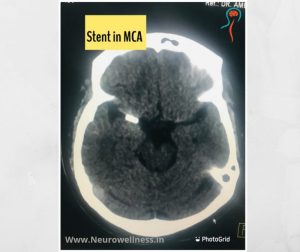
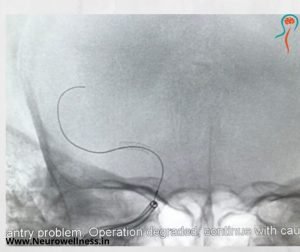
Subsequently CT angiogram and MRI scan will be performed to understand more about treatment aspect- like perfusion study.
Understanding TPA as a stroke treatment
The drug TPA is frequently used to treat ischemic strokes. It must be given to the patient within 4.5 hours after the commencement of the stroke, as permitted by the US Food and Drug Administration (FDA). There are various pros and cons to using tPA as an advanced stroke treatment in Bangalore, including the following:
Pros:
TPA can be very helpful in dissolving blood clots and increasing a patient’s chances of recovering after a stroke. At the very least, TPA may lessen the long-term repercussions of a stroke. However, the benefits of TPA are heavily dependent on when it is delivered.
Cons:
Doctor will explain everything in detail before they give blood thinners. RTPA has Bleeding risk
Summary:
Strokes are a medical emergency that requires immediate treatment.
The sooner a person receives care for a stroke, the less likely it is that permanent damage will occur.
Read more : brain stroke causes and symptoms what puts you at risk and how to spot the signs
Conclusion
Clot-busting medications like TPA (tissue plasminogen activator) have revolutionized stroke care, but timing is everything. Administering this treatment within the golden window (first 4.5 hours) can drastically reduce brain damage, prevent disability, and even save lives. The earlier the treatment, the better the outcome—making awareness and rapid action absolutely critical.
Recognizing stroke symptoms early and reaching a stroke-ready hospital immediately is the first and most important step toward recovery.
Need expert stroke care in Bangalore?
Book a consultation with Dr. Ganesh Veerabhadraiah, one of Bangalore’s top neurosurgeons.

About Author
Dr. Ganesh Veerabhadraiah
Dr. Ganesh Veerabhadraiah, leading neurosurgeon and neurologist in Bangalore, has over 20 years of expertise in managing back pain, migraines, headaches, neuro disorders, and spine problems. His clinical excellence and patient-first approach make him one of the most trusted neuro doctors in Bangalore.
At Neurowellness Brain & Spine Clinic in Jayanagar and Kavery Hospital Electronic City, Dr. Ganesh provides comprehensive treatments ranging from minimally invasive spine surgery to advanced neurological care. As a respected back pain specialist and migraine doctor, he continues to deliver reliable outcomes for patients.
👉 Connect with Dr. Ganesh on LinkedIn
FAQs
1. What is the golden hour in stroke treatment?
The golden hour is the first 60 minutes after stroke symptoms start. Quick treatment during this time with clot-busting medication can save brain cells and improve recovery.
2. Which clot-busting medication is used for stroke?
The most common clot-busting drug is tPA (tissue plasminogen activator), which helps dissolve blood clots and restore blood flow to the brain.
3. Can all stroke patients receive clot-busting treatment?
No. Eligibility depends on the type of stroke, time since symptoms began, and the patient’s medical history. A CT scan is done to confirm suitability.
4. Why is the golden hour important in stroke care?
Because “time is brain.” Each minute of delay causes brain damage. Treatment within the golden hour can reduce disability and save lives.
5. Where can I find stroke specialists in Bangalore?
You can consult experienced neurosurgeons and stroke specialists in Bangalore at Neurowellness Brain & Spine Clinic, led by Dr. Ganesh Veerabhadraiah.