Dr Ganesh Veerabhadraiah
MBBS, DNB (Neurosurgery)
FINR (Fellowship in Interventional Neurosurgery-Switzerland)
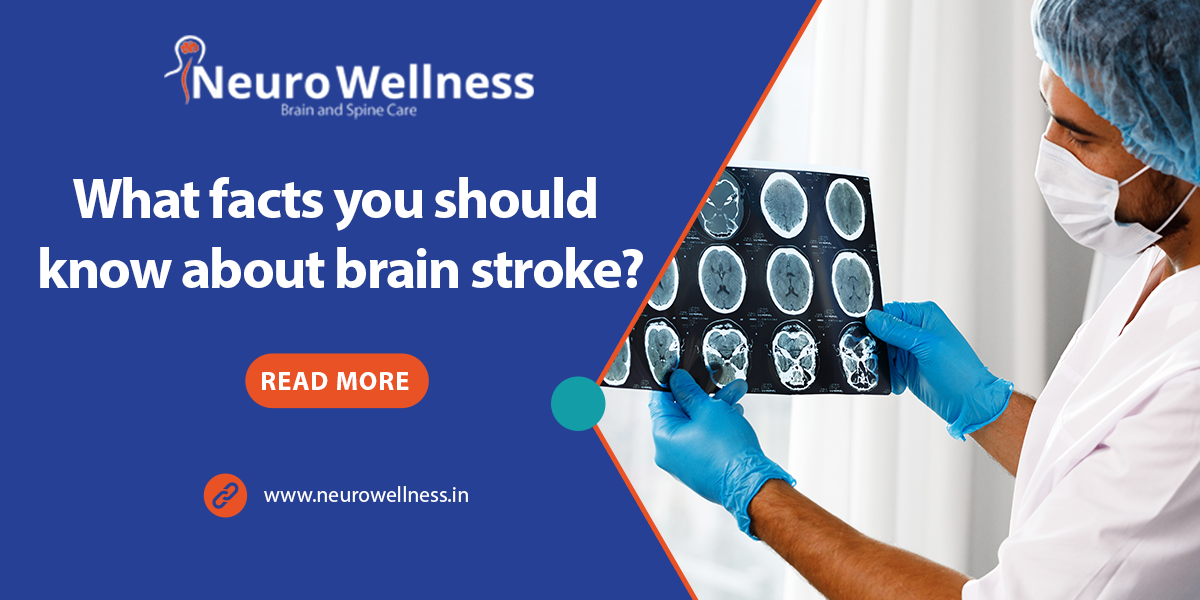
As we know about Brain Stroke: Faster you act, the better you save the patient life. National, 17th April 2022: A brain stroke, also known as a brain attack, occurs when the supply of blood to the brain is reduced or stopped. It is like a heart attack. However, in a brain stroke, due to blockage inside the vessel, blood and oxygen supply to the brain are halted. A few of the common symptoms of a brain stroke are facial weakness, arm and leg weakness, speech dysfunction, blurring of vision, and imbalance while walking. For brain stroke Dr. Ganesh Veerabhadraiah is one of the top neurosurgeon in Bangalore.
What risk factors make the brain prone to stroke?
If you are suffering from hypertension, diabetes, smoking, high cholesterol, obesity, or ischemic heart disease, you are predisposed to a brain stroke. Today’s sedentary lifestyle is one of the major causes of the development of the above-mentioned diseases, so it is important to make changes in your lifestyle so that you can keep your body healthy and reduce the risk of developing these diseases.
Do we have a golden hour in a brain stroke as we have in a heart attack?
Abrain stroke is very similar to a heart attack. Suppose a person suddenly develops chest pain, the first thing that comes to your mind is to take him or her to the hospital. As first aid, the medical team first got the ECG and ECHO done, and the cardiologist advised further treatment.
Similarly, in a brain attack or a brain stroke, complications can be avoided if the warning signs are recognized early and the person reaches the hospital within the GOLDEN HOUR.
Understand how a brain stroke happens:
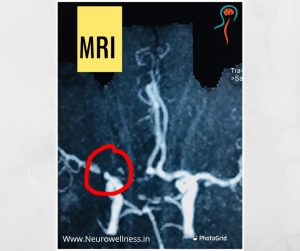
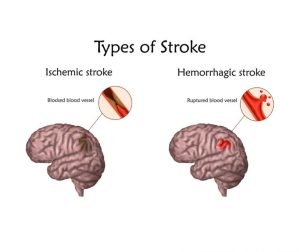
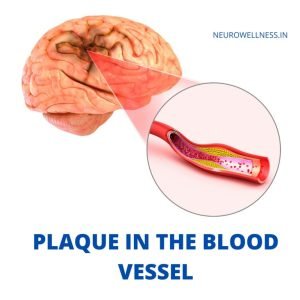
So, as we know, the heart pumps blood into the brain through blood vessels called carotid arteries, which include the right and left carotids. If there is a blockage on one side of the brain and the blood supply is hindered, it may cause a brain stroke.
Studies show that during a brain stroke, 1.9 million neurons die every minute. This happens due to a lack of blood supply and if not treated immediately it might cause permanent damage to the important parts of the brain.
A brain stroke is further classified into two categories: mini-strokes and major strokes, based on the severity and the impact it causes on the brain.
If a person suffers mini strokes, his or her condition usually improves within 24 hours, while if a person suffers from a major stroke, he or she may take longer to recover. A major stroke might also result in weakness or neurological disorders for a longer time and sometimes permanent disability. To give you entire details and the best treatment Dr. Ganesh is one of the best Neurosurgeon in Bangalore with many years of experience.
What is this golden hour of Brain Stroke: Faster you act, the better you save the patient life?
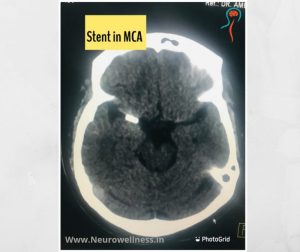
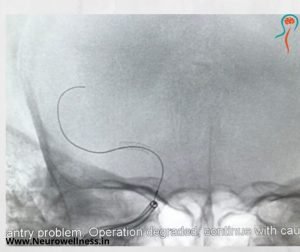
When a brain stroke happens, it is imperative to take the patient to the hospital within the golden period. The golden hour is 3.5 hours to 7.2 hours after the person has suffered a brain stroke. If the clot-bursting medication and mechanical thrombectomy happen within this period, blood circulation re-establishes. Once blood circulation is restored, the supply of blood and nutrition will again resume, which will eventually result in lowering the risk of neuronal death. This is possible with stent retrievers. It is a basket-like device. The procedure is called “Mechanical Thrombectomy.”
Mechanical thrombectomy is a new modality of interventional stroke treatment where mechanical force is applied to remove the clot by aspiration or by approaching through a basket-like device (stent retriever).
Treatment of Brain Stroke –
In recent years, comprehensive stroke treatment units have been helping people who are affected by stroke, and maximum recovery has been recorded. A comprehensive stroke unit or team consists of an emergency physician, a neurosurgeon, a neurologist, a neuroendovascular surgeon/interventional neuroradiologist, a neuro intensivist, a neuroradiologist, a neuro anaesthetist, and a physiotherapist.
Before advanced stroke treatment or endovascular stroke treatment came into the picture, conservative treatment was the only option. Patients who underwent this treatment suffered side effects or died. Usually, after this treatment, patients suffer from problems like permanent weakness in the hands and legs, speech dysfunction, persistent vegetative state, high morbidities such as the high probability of self-dependency on a wheelchair or stretcher, and long-term reliance on family, development of bedsores and sepsis, and death. If you are looking for advanced Neurosurgery in Bangalore, then Neuro Wellness is one of the best options to get the best treatment.
However, with advanced stroke treatment, patients can recover faster and better without any complications. But it will happen only if the patient comes within the golden hour. If any patient comes after the golden hour period, the right treatment cannot be started.
On seeing symptoms like facial weakness, arm or leg weakness, or speech dysfunction, to name a few, the patient should be rushed to the hospital immediately without any delay, since every second counts.
(Dr Ganesh Veerabhadraiah is Consultant – Neurosurgeon at NeuroWellness – the best neurosurgeon in Bangalore, Jayanagar 9th Block, Bengaluru. For more details visit www.neurowellness.in )