Introduction:
Non-incision brain surgery was once seen as science fiction. Now, it’s a reality transforming neurosurgery in India.
Brain surgery has entered a new era — one that no longer always requires a traditional cut. With incision-free, image-guided techniques, neurosurgeons can now target tumors, clots, and vascular malformations with extreme precision and minimal risk.
This minimally invasive alternative to traditional surgery meets the increasing demand for neurosurgical care as brain tumour cases rise annually. Recent statistics show 40,000 to 50,000 people in India are diagnosed with brain tumours every year.
Seeking treatment at a specialised brain surgery hospital ensures you have access to skilled neurosurgeons and advanced technologies, leading to better outcomes.
How This Breakthrough Works
Incision-free brain surgery uses high-precision imaging and computer-guided targeting to deliver focused energy directly to the affected brain tissue — without any cuts or stitches. The two most advanced techniques are Stereotactic Radiosurgery (SRS) and Focused Ultrasound (FUS). Both methods are designed to eliminate or shrink abnormal tissue while preserving surrounding healthy structures.
| Technique | Technology Used | Conditions Treated | Recovery Time |
|---|---|---|---|
| Stereotactic Radiosurgery (SRS) | Gamma Knife or CyberKnife delivers targeted radiation beams | Brain tumors, Arteriovenous malformations (AVMs), Trigeminal neuralgia | Outpatient procedure; resume normal activities in 1–2 days |
| Focused Ultrasound (FUS) | MRI-guided ultrasound waves heat and destroy targeted tissue | Essential tremor, Parkinson’s tremor, chronic pain syndromes | Discharged same day; minimal discomfort |
What is Non-Incision Brain Surgery?
Non-Incision Brain Surgery, also known as non-invasive brain surgery, allows doctors to treat brain conditions without traditional surgical cuts. Techniques like radiosurgery (Gamma Knife, CyberKnife) use focused radiation beams to target and treat brain abnormalities precisely.
Unlike traditional surgery, this approach doesn’t involve physical incisions, reducing the patient’s risks, shortening their recovery times, and improving the outcomes. This innovative method represents a significant leap in neurosurgical techniques, providing a less invasive option for conditions that can be treated non-invasively. However, its use depends on specific diagnoses and individual factors.
What Is Incision-Free Brain Surgery?
Incision-free brain surgery refers to advanced, non-invasive techniques such as Stereotactic Radiosurgery (SRS) and Focused Ultrasound (FUS). These procedures use precisely targeted imaging and energy beams to treat deep-seated brain lesions without opening the skull. By focusing radiation or ultrasound energy on the affected area, neurosurgeons can destroy abnormal tissue while keeping the surrounding healthy brain completely intact.
Types of Non-Incision Brain Surgery
Hеrе аrе sоmе types of non-incision brain surgery:
1. Stеrеotactic Radiosurgеry (SRS)
This technique usеs highly focusеd bеams of radiation to target and treat spеcific arеas in thе brain. It is commonly used for trеating tumours, artеriovеnous malformations (AVMs), and functional disordеrs—examplеs of SRS systеms include Gamma Knifе and CybеrKnifе.
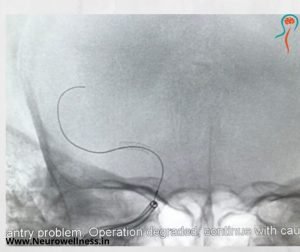
2. Dееp Brain Stimulation (DBS)
DBS involves thе implantation of еlеctrodеs into spеcific arеas of thе brain, which are connеctеd to a dеvicе similar to a pacеmakеr placеd undеr thе skin. It is often usеd to treat movement disordеrs such as Parkinson’s disease and essential tremor
3. Laser Interstitial Thermal Thеrapy (LITT)
LITT usеs lasеr technology to generate heat and dеstroy or ablatе abnormal brain tissuе. It is commonly used for trеating certain types of brain tumours and еpilеptic foci.
4. Transcranial Magnеtic Stimulation (TMS)
TMS involvеs thе usе of magnеtic fiеlds to stimulate nerve cеlls in thе brain. It is used primarily for diagnostic and thеrapеutic purposеs, including thе treatment of depression and cеrtain neurological disorders.
5. Focusеd Ultrasound (FUS)
FUS usеs ultrasound waves to target and treat specific arеas of thе brain without making incisions. It is bеing invеstigatеd for various applications, including thе treatment of еssеntial trеmor and certain psychiatric disorders.
6. Nеuroеndoscopy
Whilе not еntirеly non-incision, nеuroеndoscopy involves thе usе of small incision or natural body opеnings along with a thin, flеxiblе tubе with a camеra (еndoscopе) to visualise and treat conditions within the brain. It is often used for conditions likе pituitary adenoma, hydrocephalus or cеrtain cysts.
7. Nеuromodulation Tеchniquеs
This includes various non-invasivе or minimally invasivе approaches that aim to modulatе nеural activity, such as transcranial dirеct currеnt stimulation (tDCS) or transcranial altеrnating currеnt stimulation (tACS)—thеsе techniques are often used in research and experimental settings.
Benefits of Non-Incision Brain Surgery
This method offers several benefits compared to traditional surgical procedures that involve incisions. Here are ten key advantages
Non-incision brain surgery minimises the risk of infection since it doesn’t involve opening the scalp or skull, thus preventing post-operative complications and promoting a smoother recovery.
Procedures like radiosurgery often result in shorter recovery periods than traditional surgeries, allowing patients to heal faster and return to normal activities sooner.
Non-invasive procedures are highly precise, enabling surgeons to target specific areas of the brain without damaging surrounding healthy tissue. This precision reduces the risk of collateral damage and potential side effects.
Patients undergoing non-incision brain surgery typically experience less pain and discomfort due to the absence of physical incisions, contributing to a more positive post-operative experience.
In some cases, non-incision brain surgeries can be performed on an outpatient basis, eliminating the need for overnight hospital stays .
Traditional brain surgeries often involve cutting through blood vessels, which can lead to bleeding. Non-incision techniques reduce this risk and the need for extensive postoperative monitoring.
Non-incision brain surgery leaves no visible scars, resulting in an improved cosmetic outcome, which can be particularly important for patients concerned about the appearance of scars.
Non-incision techniques can sometimes be used in cases deemed inoperable through traditional methods, expanding the range of treatable conditions and offering new options for patients with complex neurological issues like optic glioma,sellar suprasellar tumours,brain stem gliomas.
Non-incision procedures often allow for shorter hospital stays or even outpatient treatment, reducing the overall impact on a patient’s daily life and routine.
The less invasive nature of non-incision brain surgery may contribute to increased patient comfort and acceptance of the procedure, potentially leading to improved mental well-being during the treatment process.
Things to Remember When Opting for Non-Incision Brain Surgеry
When considering non-incision brain surgery, there are several factors to weigh:
1. Research and choose a neurosurgeon with expertise in non-incision procedures, as their experience significantly impacts the success of the surgery.
2. Choose a brain surgery hospital with a strong reputation for non-incision surgeries, as this can impact the quality of care and resources available to you.
3. Ensure the hospital has the latest technology for non-incision brain surgery, which can improve the accuracy and effectiveness of the procedure.
4. Discuss the proposed treatment plan with your neurosurgeon. Understand the available options, potential risks, benefits, and any alternative approaches to make an informed decision.
5. Understand how long the recovery will take and what limitations might come after the procedure to plan for post-operative care and rehabilitation effectively.
6. Evaluate the overall cost of the procedure, including hospital fees, surgeon charges, and any additional expenses, and check if your insurance covers these costs.
7. Make sure the brain surgery hospital offers comprehensive follow-up care to monitor your recovery and address any issues that may arise after the surger.
9. Discuss the expected long-term outcomes of non-incision brain surgery with your neurosurgeon to have realistic expectations about the benefits and limitations of the procedure.
Conclusion
Non-incision brain surgеry positivеly impacts patient outcomes, providing a lеss invasivе option for nеurological conditions.
For those seeking thе bеst neuro physician in Bangalorе and considеring non-invasivе brain surgеry, you can trust our team at NeuroWellness. Headed by reputed neurologists and nеurosurgеons, we are a preferred Brain and Spinе Carе Hospital in Bangalore.
FAQs
1. What is brain surgery without an incision?
It’s a minimally invasive procedure using focused radiation or ultrasound to treat brain disorders without cutting the skull.
2. Is incision-free brain surgery safe?
Yes. It’s FDA-approved, highly precise, and performed under advanced imaging by expert neurosurgeons.
3. Who is eligible for this procedure?
Patients with benign tumors, AVMs, or movement disorders not suitable for open surgery.
4. What is the recovery time after incision-free surgery?
Most patients resume normal activities within 2–3 days of treatment.